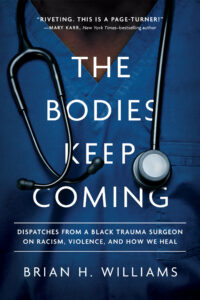
An adapted excerpt from The Bodies Keep Coming: Dispatches from a Black Trauma Surgeon on Racism, Violence, and How We Heal (Broadleaf Books)
I did not plan to become a doctor. It did not occur to me that I, a loner with an intense stare and a disheveled afro, could become a doctor like the elderly white male doctors who cared for me. As a youth I saw no one who looked like me dressed in a long white coat adorned with a stethoscope.
One of my earliest childhood memories is the feeling of impending death from lack of oxygen. “You’ll be all right, Brian,” my mother consoled, eyeing me in the rearview mirror. Wheezing like a tortured seal, I bobbled my head in acknowledgment, unable to move enough air through my lungs to speak. My father, a career Air Force noncommissioned officer, was deployed to some unknown locale, so my mother piloted this run to the hospital on her own. “You’re gonna be okay. We’ll be there soon.” I hungered for air, and seconds seemed like hours, but I knew she’d get me there. She always did. Living on an Air Force base, we didn’t have far to go, and minutes after burning rubber from home, we scurried into the emergency room.
 After the usual routine — a breathing treatment to loosen the vice grip on my lungs, height, weight, vitals — I sat hunched in an exam room, feet dangling two feet from the floor, as the doctor gently pressed here and felt there along my shirtless torso. Like all the doctors I visited as a child, he was an elderly white man who resembled Marcus Welby, MD, from the famous 1970s television series. And like all those doctors, he inspired my awe. As a military kid I always had access to healthcare, and I assumed that was true for everyone. To be sick and unable to see a doctor? I couldn’t fathom it.
After the usual routine — a breathing treatment to loosen the vice grip on my lungs, height, weight, vitals — I sat hunched in an exam room, feet dangling two feet from the floor, as the doctor gently pressed here and felt there along my shirtless torso. Like all the doctors I visited as a child, he was an elderly white man who resembled Marcus Welby, MD, from the famous 1970s television series. And like all those doctors, he inspired my awe. As a military kid I always had access to healthcare, and I assumed that was true for everyone. To be sick and unable to see a doctor? I couldn’t fathom it.
Because of my childhood asthma — a condition afflicting, hospitalizing, and killing Black children at a much higher rate than white children — I made many breathless trips to the emergency room. For many Black children, environmental injustice is an ever-present companion in neighborhoods located near municipal dumps, factories, and highways, resulting in increased exposure to respiratory toxins. My situation differed; my sister and I were trapped in a house with parents who smoked. I wonder if the white doctor judged my parents for that reason. Or because we were Black. Or both.
“Open up and say ahhh.” I coughed as the doctor gagged me with a popsicle stick and gasped when he placed an ice cube masquerading as a stethoscope to my back. “Cold, huh? Sorry about that.” My mother hovered, not saying a word as the man with the soothing voice in the long white coat poked and prodded while asking me about sports and school. “Well, we’re done,” the doctor said, smiling again. He gave my mother instructions about when to return to the hospital, said something to her about smoking, wished me luck in my upcoming game, and walked out.
Squirming into my shirt, I asked: “Are there any Black doctors?” A decade before Bill Cosby reigned as America’s favorite TV dad, Dr. Heathcliff Huxtable — and decades before it became known that he was drugging and sexually assaulting women — my mother smiled like any parent deflecting an uncomfortable truth. I couldn’t articulate it yet, but I felt it just the same. To me the smiling man in the long white coat, with the fancy degrees and plaques and awards broadcasting greatness from his office walls, was a god. And like the Eurocentric religious ideals force-fed to me in Sunday school, his profession of medicine did not seem like somewhere I belonged.
From that early age, I knew an unspoken truth: No matter how smart, articulate, or well-behaved I would become, there were always places Black boys would not be welcome.
Black men in medicine represent less than 3% of doctors, and I know future Black men attempting to cross the threshold are depending on Black doctors like me. Patients have told me to get their “real” doctor, leave the room, remove their tray of half-eaten food, or empty the trash bin. Some have ignored me and others have spat at me. Some have prayed for me and others have wished me dead. I have been called a racist and a healer, a nigger and a sellout, a hypocrite and a hero. No matter our social status, from gang members to doctors, Black men still serve as a mirror for people’s fears. A screen on which to project one’s anxiety — and disgust. An endangered species navigating a world both hostile to and dependent upon our existence.
Even with this backdrop, who is more poised to address the realities of our health inequities than those who have had to survive it? Childhood asthma does kill Black children at higher rates than white children. But so do other respiratory diseases, cardiovascular disease, neurological diseases. All of this ties back to environmental injustice. And those environmental injustices are inextricably linked to larger societal disparities that position Black and brown communities to be most likely affected.

As a trauma surgeon, I learned to compartmentalize. The trauma team must move on. The hospital must move on. I must be ready for another victim, arriving with lights and sirens. I file away a mother’s son’s death in the emotional lockbox, straining to contain the feelings of injustice for the countless others like him. In these moments I reckon with the role I play as a Black doctor in a society that devalues Black lives. I wrestle with the futile feeling that the nobility of my work doesn’t have a sustainable impact. Is the essence of my job plugging bullet holes in young Black men and women, or watching them unable to breathe properly, or develop healthily? I can’t help but think that the histories and policies designed to quarantine Black people from mainstream American society have somehow managed to reach across generations and plague us today.
I write and act so that other five-year-old wheezing Black boys might be seen as part of a bigger picture that needs attention. I write and act to show you the world of a Black trauma surgeon, in a profession lacking role models, who routinely deals with the human toll from the implications of environmental injustices. I write and act to remind us all that if Black lives actually mattered to policymakers in the United States, they would take action that mattered.
Previously in The Revelator:
Compounding a Crisis: When Public Health Solutions Worsen Climate Change


